Diabetes and Your Eyesight: Protecting Vision from Retinopathy
Living with diabetes requires careful management of blood sugar levels to protect your overall health. But did you know that diabetes can also significantly impact your eyesight? One of the most serious eye complications related to diabetes is Diabetic Retinopathy, a condition that damages the blood vessels in the retina, the light-sensitive tissue at the back of your eye.
For seniors managing diabetes, understanding diabetic retinopathy and taking proactive steps to prevent or manage it is crucial for preserving vision. This guide from Elderly Care First explains what diabetic retinopathy is, its stages, symptoms, risk factors, and most importantly, how seniors with diabetes can actively protect their sight.
What is Diabetic Retinopathy?
High blood sugar levels over time can damage tiny blood vessels throughout the body, including those in the retina. Diabetic retinopathy occurs when these retinal blood vessels become damaged. This damage can happen in two main stages:
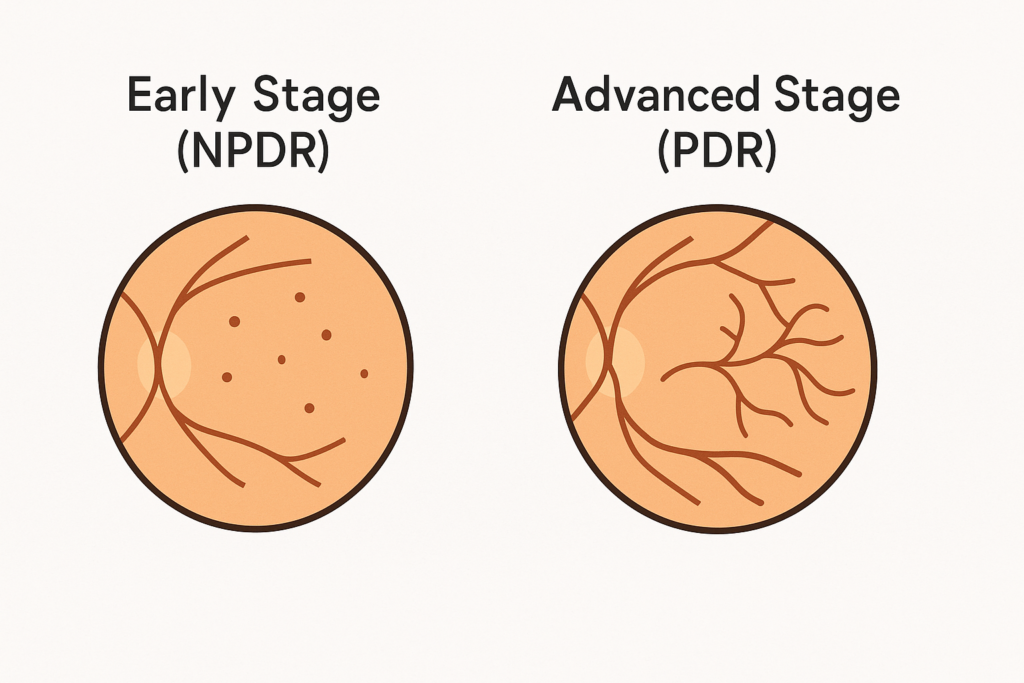
1. Non-Proliferative Diabetic Retinopathy (NPDR):
- Early Stage: In this stage, blood vessels in the retina weaken and may leak fluid or small amounts of blood, causing swelling in the retina (macular edema) or the formation of small pouches (microaneurysms).
- Symptoms: Often, there are no symptoms in the early stages of NPDR, which is why regular eye exams are vital. If macular edema occurs (swelling in the central part of the retina, the macula), vision can become blurry.
2. Proliferative Diabetic Retinopathy (PDR):
- Advanced Stage: This is a more serious stage where damaged blood vessels close off, prompting the retina to grow new, abnormal, fragile blood vessels. This process is called neovascularization.
- Complications: These new vessels are weak and can easily bleed into the vitreous (the clear gel filling the eye), causing floaters or severe vision loss. They can also form scar tissue, which can pull on the retina and potentially lead to retinal detachment – a sight-threatening emergency. These abnormal vessels can also interfere with fluid flow in the eye, sometimes leading to neovascular glaucoma, a severe type of glaucoma. Glaucoma Guide
- Symptoms: Symptoms can include blurred vision, fluctuating vision, dark spots or “cobwebs” (floaters), shadows in your field of vision, or sudden, severe vision loss.
Diabetic Macular Edema (DME): This swelling of the macula due to leaking blood vessels can occur at any stage of diabetic retinopathy (NPDR or PDR) and is a common cause of vision loss in people with diabetes. AMD Guide for context on macula
Symptoms to Watch For
While early stages often have no symptoms, be aware of potential signs as the condition progresses:
- Blurry or fluctuating vision
- Dark spots, strings, or “cobwebs” floating in your vision (floaters)
- Dark or empty areas in your field of vision
- Difficulty seeing colors
- Poor night vision
- Sudden vision loss
Don’t wait for symptoms to appear. If you have diabetes, regular comprehensive eye exams are essential for early detection.
Who is at Risk?
Anyone with diabetes (Type 1, Type 2, or gestational diabetes) is potentially at risk. Several factors increase the likelihood and severity:
- Duration of Diabetes: The longer you’ve had diabetes, the higher your risk.
- Poor Blood Sugar Control: Consistently high blood sugar levels significantly increase the risk and speed up progression.
- High Blood Pressure: Uncontrolled hypertension adds stress to blood vessels, including those in the eye.
- High Cholesterol: Can contribute to blood vessel damage.
- Pregnancy: Can sometimes worsen existing retinopathy.
- Race: African Americans, Hispanics, and Native Americans may have a higher risk of developing diabetic retinopathy.
- Smoking: Worsens circulation and increases risk.
The Critical Importance of Regular Eye Exams
Because diabetic retinopathy often has no early warning signs, seniors with diabetes should have a comprehensive dilated eye exam at least once a year, or more frequently if recommended by their eye doctor.
During this exam, the doctor will dilate your pupils to get a clear view of your retina and check for:
- Leaking blood vessels
- Retinal swelling (macular edema)
- Fatty deposits (exudates) on the retina
- Damaged nerve tissue
- Any abnormal new blood vessel growth

Early detection allows for timely treatment, which can prevent or delay severe vision loss. Medicare & Eye Exams Guide
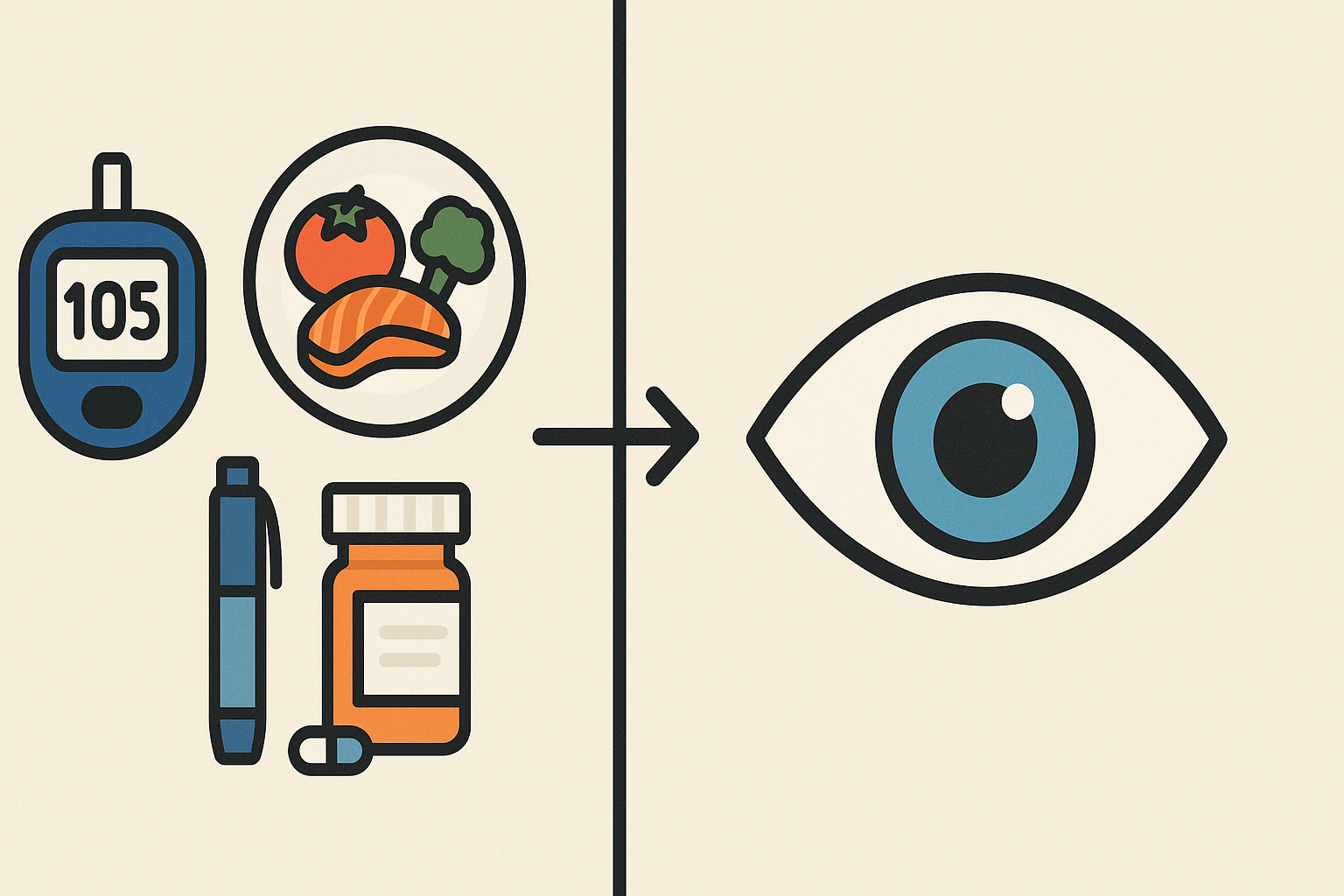
Preventing and Managing Diabetic Retinopathy

The most effective ways to protect your vision involve managing your diabetes and related health conditions:
- Control Your Blood Sugar (A1C): Work closely with your primary care doctor or endocrinologist to keep your blood sugar levels within your target range as consistently as possible. This is the single most important factor.
- Manage Blood Pressure: Keep blood pressure under control through lifestyle changes and medication if needed.
- Control Cholesterol: Maintain healthy cholesterol levels.
- Take Prescribed Medications: Adhere strictly to your diabetes, blood pressure, and cholesterol medications.
- Maintain a Healthy Lifestyle: Eat a balanced diet, get regular exercise (as approved by your doctor), and maintain a healthy weight.
- Don’t Smoke: If you smoke, seek help to quit.
- Attend Regular Eye Exams: Schedule and keep your annual (or more frequent) dilated eye exams without fail.
Treatment Options for Diabetic Retinopathy
If retinopathy progresses, treatments are available to slow or stop further damage and preserve vision:
- Anti-VEGF Injections: Similar to treatment for Wet AMD, injections of anti-VEGF medication into the eye can help reduce macular swelling (DME) and shrink abnormal blood vessels (PDR). This is often a first-line treatment.
- Laser Treatment (Photocoagulation):
- Focal Laser: Used to treat macular edema by sealing specific leaking blood vessels.
- Scatter Laser (Pan-retinal Photocoagulation – PRP): Used for PDR to shrink abnormal blood vessels throughout the peripheral retina. This can sometimes cause some loss of side vision or night vision but helps save central vision.
- Corticosteroid Injections/Implants: Steroids injected or implanted into the eye can also help reduce macular edema, though they carry risks like increased eye pressure or cataract formation.
- Vitrectomy: A surgical procedure to remove blood and scar tissue from the vitreous gel inside the eye. This may be needed for advanced PDR complications like severe bleeding or retinal detachment.
Your ophthalmologist will recommend the best treatment based on the stage and specific features of your diabetic retinopathy.
Conclusion: Take Control of Diabetes to Protect Your Sight
Diabetic retinopathy is a serious potential complication of diabetes, but it is not an inevitable consequence. By diligently managing your blood sugar, blood pressure, and cholesterol, maintaining a healthy lifestyle, and committing to regular comprehensive eye exams, seniors with diabetes can significantly reduce their risk of vision loss. Early detection and timely treatment are key to preserving your precious eyesight for years to come.
Work closely with your entire healthcare team – primary care doctor, endocrinologist (if applicable), and eye doctor – to protect both your overall health and your vision. Elderly Care First encourages you to be proactive about diabetes management and eye care.