As we age, our bodies undergo various changes, and our eyes are no exception. One of the most common age-related eye conditions seniors face is cataracts. If you or a loved one are experiencing changes in vision, understanding cataracts is the first step towards maintaining sight and quality of life. This guide provides comprehensive information about cataract symptoms, causes, diagnosis, treatments, surgery, and recovery specifically for seniors. We aim to empower you with knowledge from trusted sources, helping you navigate this common condition with confidence. Remember, while cataracts are prevalent, advancements in treatment mean vision can often be significantly restored.
What are Cataracts? Understanding the Clouding Lens
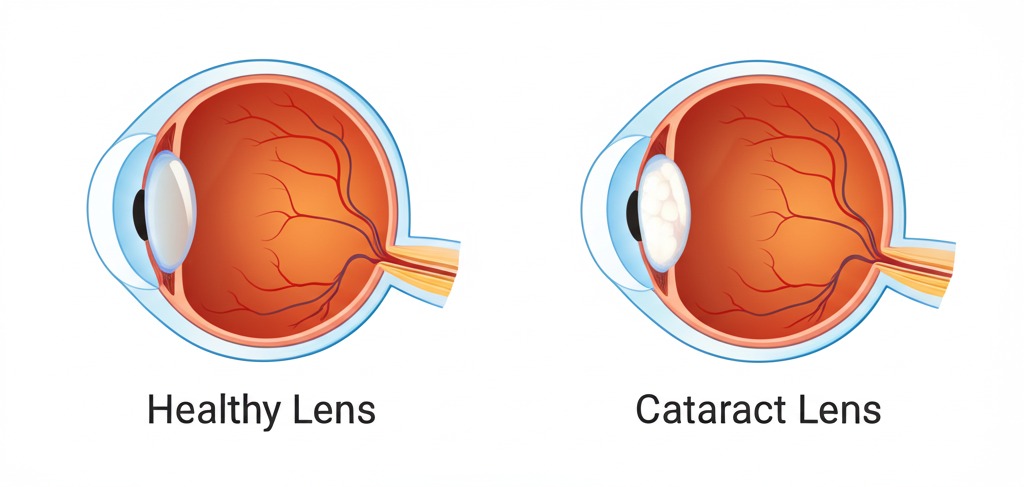
Imagine looking through a window that’s becoming progressively foggy or frosted – that’s similar to how cataracts affect vision. A cataract is a clouding of the eye’s natural lens, the clear part located behind the iris (the colored part) and pupil. The lens works much like a camera lens, focusing light onto the retina at the back of the eye, where images are processed. According to the National Eye Institute (NEI), the lens is mostly made of water and protein. As we age, some of this protein can clump together, forming a cloudy area – the cataract.
This clouding prevents light from passing clearly through the lens, causing blurred or dimmed vision. Cataracts typically develop slowly over years and don’t usually cause pain. While most cataracts are age-related, appearing in people over 60, they can occur at any age. Understanding that this is a structural change within the eye helps clarify why simple eyeglass updates eventually become insufficient as the cataract progresses. Different types exist, like nuclear (affecting the lens center), cortical (affecting the lens edges), and posterior subcapsular (affecting the back), each potentially causing slightly different symptoms initially (Source: American Academy of Ophthalmology – AAO).
Recognizing the Signs: Symptoms of Cataracts in Seniors
Because cataracts often develop gradually, seniors might initially dismiss subtle vision changes as just part of getting older or needing a new glasses prescription. However, recognizing specific symptoms is crucial for timely diagnosis. Common signs of cataracts in older adults include:
- Blurry or Cloudy Vision: This is the hallmark symptom. Vision may seem hazy, filmy, or like looking through dirty glass.
- Dimmed Colors: Colors may appear faded, less vibrant, or yellowish. Distinguishing between blues and purples might become difficult.
- Increased Glare Sensitivity: Headlights, lamps, or sunlight may seem overly bright or cause glare, especially noticeable when driving at night.
- Halos Around Lights: Seeing rings or halos around light sources.
- Poor Night Vision: Difficulty seeing in low light conditions.
- Double Vision (in one eye): Seeing multiple images out of a single eye can sometimes occur with cataracts.
- Frequent Prescription Changes: Needing increasingly frequent updates to eyeglass or contact lens prescriptions. In some cases, near vision might temporarily improve (called “second sight”), but this effect is short-lived as the cataract worsens (Source: Mayo Clinic).
If you or a senior you care for experiences any of these symptoms, scheduling an eye exam with an ophthalmologist or optometrist is essential. Early detection allows for monitoring and planning appropriate management.
Why Do Cataracts Happen? Causes and Risk Factors in Aging Eyes
The primary cause of cataracts is aging. The proteins in the eye’s lens naturally change and break down over time, leading to clouding. The NEI states that by age 80, more than half of all Americans either have a cataract or have had cataract surgery. However, certain factors can increase the risk of developing cataracts earlier or accelerate their progression:
- Age: The most significant risk factor.
- Underlying Health Conditions: Diabetes significantly increases cataract risk. Hypertension may also play a role.
- Excessive Sun Exposure: Prolonged exposure to ultraviolet (UV) radiation from the sun can contribute to cataract formation.
- Smoking: Smoking doubles the risk of developing cataracts compared to non-smokers.
- Previous Eye Injury or Surgery: Trauma or prior intraocular surgery can increase risk.
- Long-term Steroid Use: Prolonged use of corticosteroid medications (oral, inhaled, or eye drops) is linked to cataract development.
- Family History: Having family members with cataracts may increase your own risk.
- Poor Nutrition: Some studies suggest antioxidant vitamins and minerals might play a protective role, implying deficiencies could increase risk, though more research is needed (Source: AAO).
- Excessive Alcohol Consumption: Heavy drinking may also increase cataract risk.
Understanding these risk factors highlights the importance of lifestyle choices, managing health conditions, and protecting your eyes throughout life.
Getting a Clear Picture: How Cataracts are Diagnosed

Diagnosing cataracts involves a comprehensive eye examination by an eye care professional (ophthalmologist or optometrist). If you suspect cataracts, the doctor will likely perform several tests:
- Visual Acuity Test: This standard eye chart test measures how well you see at various distances. It helps quantify the degree of vision impairment.
- Slit-Lamp Examination: This uses a special microscope with a bright light (slit lamp) to examine the structures at the front of your eye – the cornea, iris, and lens – in detail. The magnification allows the doctor to detect even small opacities in the lens, confirming the presence and assessing the density of a cataract.
- Retinal Exam (Fundoscopy): The doctor will likely dilate your pupils using eye drops. This widens the pupil, providing a better view of the lens and the retina at the back of the eye. This helps rule out other conditions that could be causing vision problems, such as glaucoma or macular degeneration, and allows assessment of the cataract’s impact on the view of the retina (Source: AAO).
These painless tests allow the doctor to confirm a cataract diagnosis, determine its severity, and discuss how it might be affecting your daily activities and quality of life. Regular eye exams are crucial for seniors, even without symptoms, as they allow for early detection.
Managing Cataracts: Treatment Options Available
Once diagnosed, the treatment approach for cataracts depends on how much they impact your vision and daily life.
Non-Surgical Treatments & Management
In the early stages, when vision changes are mild, surgery might not be immediately necessary. Non-surgical strategies can help manage symptoms:
- Updated Eyeglass Prescription: Ensuring your glasses or contact lenses are the correct strength can improve vision temporarily. Bifocals or progressive lenses might be helpful.
- Improved Lighting: Using brighter reading lamps or increasing ambient light at home can make tasks easier. Task lighting directed onto reading material or crafts is often beneficial.
- Anti-Glare Sunglasses: Wearing sunglasses that block UV rays and reduce glare can improve comfort outdoors. Polarized lenses are particularly effective.
- Magnifying Lenses: Using handheld or stand magnifiers can assist with reading fine print or hobbies.
It’s important to understand, as the NEI points out, that these measures do not slow down or reverse cataract development. They simply help you cope with the symptoms. Eventually, as the cataract progresses and significantly impairs vision, surgery becomes the only effective treatment.
Surgical Treatments: The Definitive Solution
Cataract surgery is one of the most common and successful surgical procedures performed worldwide. It involves removing the clouded natural lens and replacing it with a clear, artificial intraocular lens (IOL).
- Traditional Cataract Surgery (Phacoemulsification): This is the most common method. The surgeon makes a very small incision in the cornea (the clear front part of the eye). A tiny probe emitting ultrasonic waves is inserted to break up (emulsify) the cloudy lens, which is then gently suctioned out. The IOL is then folded, inserted through the same incision, and unfolded into place. Often, the incision is self-sealing and requires no stitches (Source: AAO).
- Laser-Assisted Cataract Surgery (FLACS): This technique uses a femtosecond laser for certain steps traditionally done manually. The laser can create precise corneal incisions, open the lens capsule (capsulotomy), and soften/fragment the cataract, potentially allowing for less ultrasound energy use during removal. While FLACS offers high precision, studies haven’t consistently shown significantly better visual outcomes compared to expertly performed traditional surgery for all patients. Your surgeon can discuss if FLACS offers specific advantages for your situation (Source: AAO).
The choice between traditional and laser-assisted surgery depends on factors like surgeon preference, technology availability, cost (FLACS often involves additional out-of-pocket expenses), and individual eye characteristics.
Cataract Surgery for Seniors: What to Expect
The prospect of eye surgery can be daunting, especially for seniors or those caring for them. However, understanding the process can alleviate anxiety. Cataract surgery is typically an outpatient procedure, meaning you go home the same day.

Procedure Overview (Simplified)
- Numbing: Your eye will be numbed with anesthetic eye drops or an injection around the eye. You may also receive mild sedation to help you relax, but you’ll remain awake.
- Incision: The surgeon makes tiny incisions in the cornea.
- Opening the Capsule: A circular opening is made in the thin membrane (capsule) surrounding the lens. (This can be done manually or with a laser in FLACS).
- Removing the Cataract: Using ultrasound (phacoemulsification) or laser fragmentation followed by suction, the cloudy lens material is removed. The back membrane of the capsule is left intact to support the new lens.
- Inserting the IOL: The artificial intraocular lens (IOL) is folded and inserted through the incision into the lens capsule.
- Closing: The corneal incisions are usually self-sealing but may occasionally require a single stitch. A protective shield is typically placed over the eye.
The entire procedure usually takes only 10-20 minutes per eye. If both eyes need surgery, they are typically done several weeks apart.
Preparing for Surgery: A Practical Caregiver Checklist

Preparation is key for a smooth experience. Caregivers play a vital role. Here’s a checklist:
- Understand Pre-Op Instructions: Ensure the patient (and you) fully understand the surgeon’s instructions regarding eating/drinking restrictions before surgery and any medications to stop or continue (especially blood thinners). Note any pre-operative eye drop schedules.
- Arrange Transportation: The patient cannot drive immediately after surgery. Arrange reliable transport to and from the surgical center and for the first post-op appointment (usually the next day).
- Plan for Post-Op Eye Drops: Cataract surgery requires diligent use of prescribed antibiotic and anti-inflammatory eye drops for several weeks to prevent infection and reduce swelling. Create a clear schedule, perhaps using alarms or a chart. Assist the senior if they have difficulty administering drops themselves due to arthritis or unsteadiness. Many caregivers find setting phone reminders or using a simple daily checklist very helpful for managing the drop schedule.
- Prepare Easy Meals: Have simple, easy-to-prepare meals ready for the first few days post-surgery, as the patient will be advised to rest and avoid strenuous activity.
- Home Environment: Ensure pathways are clear to prevent falls while vision might be adjusting or if an eye shield is worn. Have sunglasses ready for increased light sensitivity.
- Medication List: Have an updated list of all medications (including over-the-counter and supplements) ready for the surgical team.
- Comfort Items: Have pain relievers (like acetaminophen, as advised by the doctor), comfortable pillows for resting, and perhaps audiobooks or music available.
- Know Who to Call: Have the surgeon’s office number readily available for any questions or concerns.
“Good preparation significantly reduces anxiety for both the patient and the family,” notes Dr. Emily Carter, an ophthalmologist specializing in geriatric eye care. “Knowing what to expect and having support systems in place makes the highly successful process of cataract surgery even smoother.“
Smooth Sailing: Recovery & Understanding Common Complications

Recovery from cataract surgery is generally quick, with most seniors noticing improved vision within a few days. However, following post-operative instructions carefully is crucial for optimal healing and avoiding complications.
Post-Surgery Recovery Tips & Timeline
- Immediately After: You’ll rest briefly at the surgical center before going home. Vision might be blurry initially due to dilation, anesthetic, and mild swelling. Wear the protective eye shield as instructed, especially while sleeping, usually for the first week.
- First Few Days:
- Use prescribed eye drops exactly as directed.
- Avoid rubbing or pressing on the eye.
- Wear sunglasses outdoors or in bright light.
- Light activities like reading or watching TV are usually fine.
- Avoid bending over deeply, strenuous lifting (typically over 10-15 lbs), and activities that could cause jolting or impact to the head/eye.
- Showering/bathing is usually okay, but avoid getting soap or water directly into the eye. Don’t swim or use hot tubs.
- First Few Weeks:
- Attend all follow-up appointments. The doctor will monitor healing and check vision.
- Continue eye drops for the prescribed duration (often 3-4 weeks, tapering off).
- Gradually resume normal activities as advised by your surgeon. Restrictions on strenuous activities may last several weeks.
- Your vision will continue to stabilize. A final eyeglass prescription (if needed, often just for reading if a monofocal IOL was used) is usually determined about 4-6 weeks post-surgery (Source: NEI).
Common Complications & When to Seek Help
While cataract surgery has a high success rate (over 95% according to the AAO), minor complications can occur, and recognizing them is important. Most are treatable:
- Inflammation/Swelling: Some degree is normal, managed with anti-inflammatory drops. Excessive or prolonged inflammation needs assessment.
- Infection (Endophthalmitis): Rare but serious. Signs include increasing redness, pain, discharge, and decreased vision. Requires immediate medical attention. Diligent use of antibiotic drops minimizes this risk.
- Increased Eye Pressure: Can occur temporarily, usually managed with drops.
- Posterior Capsular Opacification (PCO): Sometimes called a “secondary cataract,” this is common months or years after surgery. The back part of the lens capsule (left intact during surgery) becomes cloudy. Symptoms mimic the original cataract (blurry vision). It’s easily treated with a quick, painless laser procedure (YAG capsulotomy) in the office (Source: Mayo Clinic).
- Retinal Detachment: A rare complication, more common in highly nearsighted individuals or those with previous eye issues. Symptoms include sudden flashes of light, floaters, or a curtain-like shadow over vision. Requires urgent attention.
Contact your eye surgeon immediately if you experience:
- Severe or worsening eye pain
- Significant decrease in vision
- Sudden onset of flashing lights or many new floaters
- Increased redness or discharge from the eye
Prompt attention to these warning signs is crucial for managing potential issues effectively.
Protecting Your Sight: Prevention & Lifestyle Tips

While age-related cataracts cannot be entirely prevented, certain lifestyle measures may help slow their progression or reduce risk:
- Wear UV-Protective Sunglasses: Choose sunglasses that block 100% of UVA and UVB rays whenever you’re outdoors. A wide-brimmed hat adds extra protection.
- Don’t Smoke: Smoking significantly increases cataract risk. Quitting offers numerous health benefits, including for your eyes. Resources are available to help you quit.
- Eat a Healthy Diet: Include plenty of fruits and vegetables rich in antioxidants (like vitamins C and E). Leafy greens, colorful produce, and fish high in omega-3 fatty acids support overall eye health (Source: AAO, AREDS studies).
- Manage Health Conditions: Keep diabetes and hypertension under control through medication, diet, and exercise as recommended by your doctor.
- Moderate Alcohol Intake: Limit alcohol consumption.
- Regular Eye Exams: Crucially, schedule comprehensive dilated eye exams regularly (annually for seniors over 65, or as recommended by your eye doctor). This allows for early detection and monitoring of cataracts and other age-related eye conditions like glaucoma and macular degeneration.
Enhancing Vision: Best Vision Aids & Products for Seniors with Cataracts

For seniors whose cataracts aren’t yet severe enough for surgery, or for those with residual vision needs even after surgery (e.g., needing reading glasses), various aids can significantly improve daily functioning:
- Proper Lighting: Good illumination is key. Use flexible task lamps for reading or hobbies. Ensure rooms are well-lit, minimizing glare where possible (e.g., using lampshades, avoiding bare bulbs).
- Magnifiers: Handheld, stand, or electronic magnifiers (video magnifiers) can enlarge text and objects, making reading and detailed tasks easier. Options range from simple magnifying glasses to sophisticated digital devices.
- Large Print Materials: Books, playing cards, keyboards, and phone dials are available in large print formats. Adjusting font sizes on computers, tablets, and smartphones can also help.
- High-Contrast Items: Using items with high contrast (e.g., black marker on white paper, white mug for dark coffee) can improve visibility.
- Assistive Technology: Smartphone apps offer magnification, text-to-speech functions, and other visual aids. Smart home devices can control lighting with voice commands.
An optometrist specializing in low vision can provide personalized recommendations for aids and strategies based on individual needs and the degree of vision impairment.
Conclusion: Clearer Sight, Brighter Future
Cataracts are a common part of aging for many seniors, but they don’t have to mean permanent vision loss or a diminished quality of life. Understanding the symptoms allows for early detection through regular eye exams. While non-surgical options can help manage early stages, modern cataract surgery offers a safe and highly effective way to restore clear vision. With excellent success rates and generally quick recovery times, surgery can significantly improve independence, safety (especially regarding falls and driving), and enjoyment of daily activities. By staying informed, working closely with your eye care team, and utilizing available resources and aids, seniors facing cataracts can look forward to a brighter, clearer future.
Don’t let cloudy vision dim your world. If you suspect cataracts or haven’t had a recent eye exam, schedule an appointment with your eye doctor today to discuss your vision health and options.
Disclaimer: This blog post provides general information and discussions about health and related subjects. The information and other content provided in this blog post, or in any linked materials, are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







3 Comments