Understanding Age-Related Macular Degeneration (AMD)
As we get older, changes in our vision are common. One condition that significantly affects eyesight in seniors is Age-Related Macular Degeneration, often called AMD. It’s a leading cause of vision loss for people over 60, primarily impacting the sharp, central vision needed for tasks like reading, driving, and recognizing faces.
Hearing a diagnosis of AMD can be concerning, but it’s important to know that AMD does not usually cause complete blindness. While it affects central vision, peripheral (side) vision typically remains. Understanding AMD is the first step towards managing it effectively and maintaining your quality of life. This guide from Elderly Care First explains AMD in simple terms for seniors and their caregivers.
What Exactly is AMD?
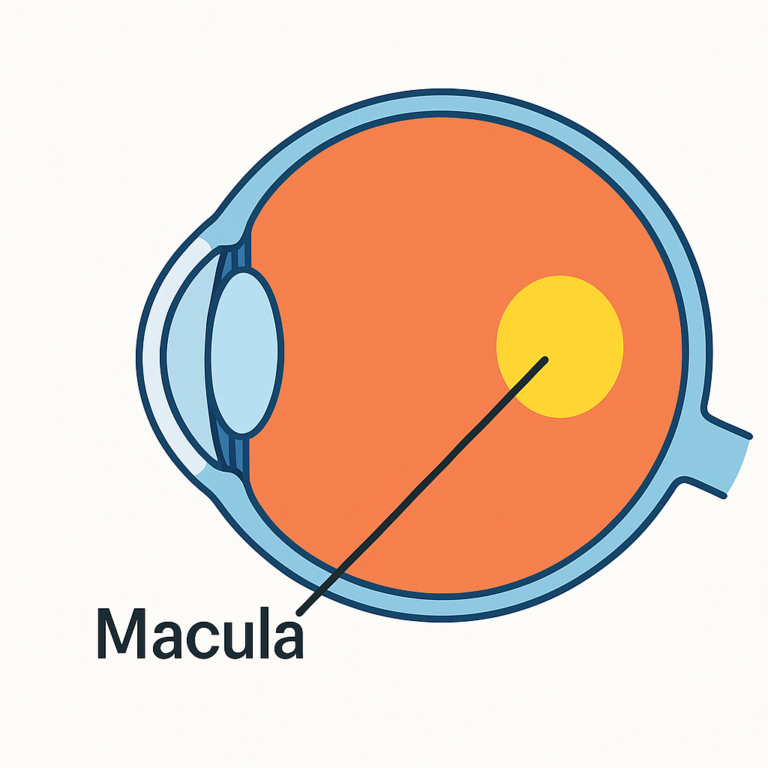
Imagine your eye is like a camera. The retina, at the back of the eye, acts like the camera’s film, capturing images. In the center of the retina is a tiny area called the macula. The macula is responsible for your sharpest, most detailed central vision.
Age-Related Macular Degeneration (AMD) occurs when this crucial macula area becomes damaged or starts to break down. This damage makes it harder to see fine details clearly, both up close and far away.
The Two Types of AMD: Dry vs. Wet
AMD comes in two main forms:
1. Dry AMD (Atrophic AMD)
- More Common: This is the most frequent type, accounting for about 80-90% of all AMD cases.
- Gradual Changes: It usually progresses slowly over many years. It happens as the light-sensitive cells in the macula gradually thin and break down, and tiny yellow deposits called drusen build up under the retina.
- Symptoms: Vision loss is typically gradual. You might notice needing brighter light to read, colors seeming less vibrant, or a slightly blurry spot in your central vision.
2. Wet AMD (Neovascular AMD)
- Less Common, More Severe: Although less frequent, Wet AMD is responsible for most cases of severe vision loss from AMD.
- Rapid Changes: It can develop suddenly and progress quickly. It occurs when abnormal, fragile blood vessels grow underneath the macula. These vessels can leak blood and fluid, causing scarring and rapid damage to the macula.
- Symptoms: Vision changes are often more sudden and noticeable. Straight lines may appear wavy or distorted, and a distinct blurry or blind spot can appear in the central vision. Wet AMD is considered a medical urgency requiring prompt attention from an eye doctor.
It’s possible for Dry AMD to progress to Wet AMD over time.
Symptoms of AMD to Watch For
Because AMD affects central vision, symptoms often involve difficulty with detailed tasks. Be aware of:
- Blurry or fuzzy central vision: Difficulty seeing details clearly, like words on a page or faces.
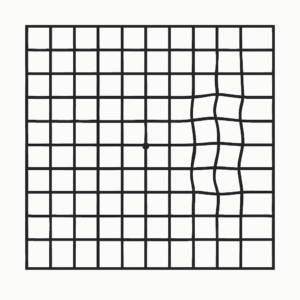
- Straight lines appearing wavy or distorted: This is a key sign, especially of Wet AMD. Using an Amsler grid (a simple chart with lines) can help detect this.
- Blurry or fuzzy central vision: Difficulty seeing details clearly, like words on a page or faces.
- Straight lines appearing wavy or distorted: This is a key sign, especially of Wet AMD. Using an Amsler grid (a simple chart with lines) can help detect this.
- A dim or dark spot in the center of your vision.
- Needing brighter light for reading or close work.
- Difficulty adapting from bright light to low light.
- Colors seeming less bright or vivid than they used to.
- Trouble recognizing familiar faces.
If you notice any of these symptoms, especially sudden changes or wavy lines, see an eye doctor right away.
Who is at Risk for AMD?
While age is the biggest risk factor, other things can increase your chances of developing AMD:
- Age: Risk increases significantly after age 60.
- Smoking: Smoking doubles or even triples the risk of AMD.
- Family History: Having a close relative with AMD increases your risk.
- Race: Caucasians have a higher risk compared to other racial groups.
- Diet: Diets low in certain nutrients (like leafy greens) may increase risk.
- Cardiovascular Health: High blood pressure and heart disease may be linked to AMD.
How is AMD Diagnosed?
AMD is usually detected during a comprehensive dilated eye exam. Your eye doctor will:
- Check Your Vision: Using an eye chart.
- Examine Your Retina and Macula: After dilating your pupils (using drops to widen them), the doctor uses special lenses to look at the back of your eye for signs of drusen or damage.
- Amsler Grid Test: You may be asked to look at a grid pattern to check for wavy lines or blind spots.
- Other Tests (if needed): If Wet AMD is suspected, tests like Optical Coherence Tomography (OCT – creates cross-section images of the retina) or Fluorescein Angiography (injecting dye to see blood vessel leakage) might be done.
Treatment Options for AMD
While there’s currently no cure for AMD, treatments can help slow its progression, especially for Wet AMD, and help people manage vision loss.
- Dry AMD Treatment:
- AREDS 2 Vitamins: For people with intermediate or advanced Dry AMD in one eye, specific high-dose vitamin and mineral supplements (based on the Age-Related Eye Disease Studies – AREDS/AREDS2) may help slow down the progression. Consult your eye doctor before starting any supplements.
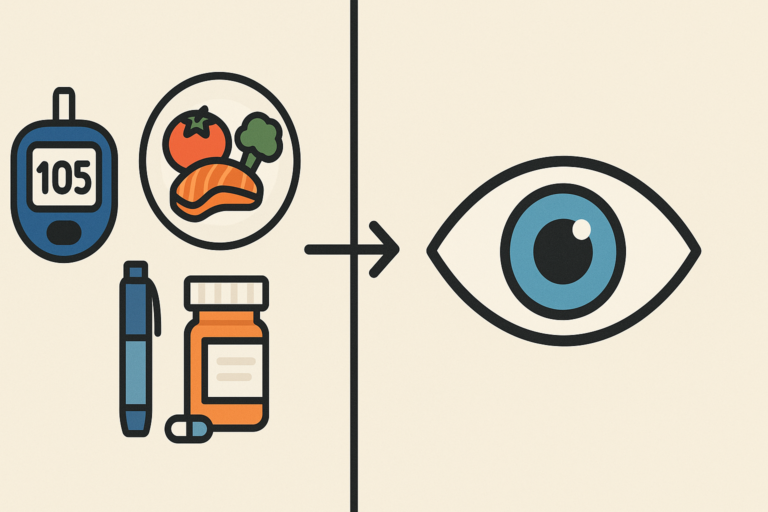
- Lifestyle Changes: Quitting smoking, eating an eye-healthy diet, and protecting eyes from UV light are often recommended.
- Wet AMD Treatment:
- Anti-VEGF Injections: The main treatment involves regular injections of medication directly into the eye. These drugs block a substance called Vascular Endothelial Growth Factor (VEGF), which promotes abnormal blood vessel growth. This can stop leakage, reduce swelling, and sometimes improve vision.
- Photodynamic Therapy (PDT): Less commonly used now, this involves injecting a light-sensitive drug and using a laser to close leaking vessels.
Treatments aim to preserve existing vision and prevent further loss.
Living Well with AMD
Even with vision changes, strategies and tools can help you adapt and maintain independence:
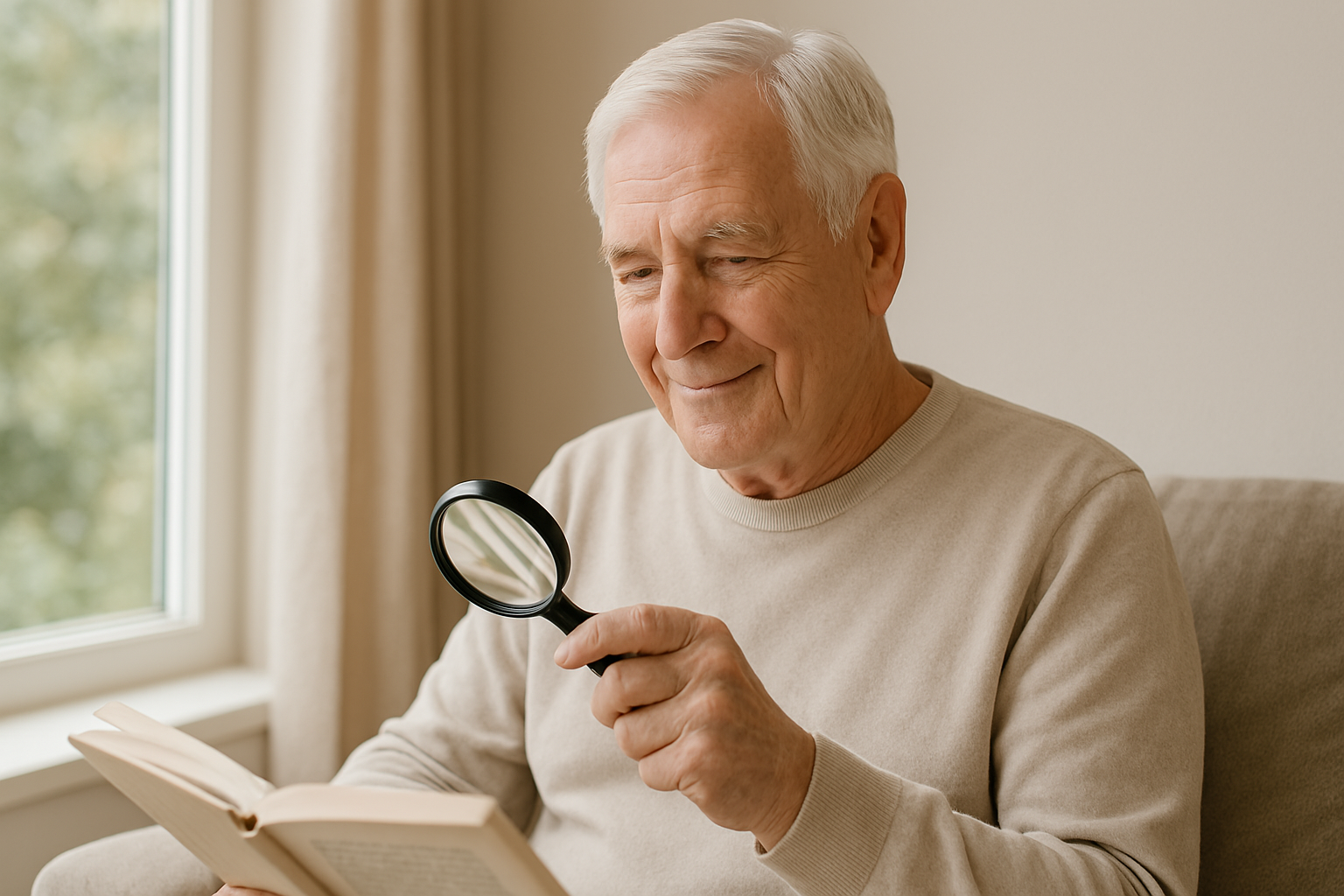
- Use Magnifiers: Handheld, stand, or electronic magnifiers can make reading and close tasks easier.
- Improve Lighting: Ensure good, bright, targeted lighting for tasks, avoiding glare.
- Low Vision Aids: Explore large-print books, phones with large buttons, talking clocks, and computer software that enlarges text or reads it aloud.
- Low Vision Aids: Explore large-print books, phones with large buttons, talking clocks, and computer software that enlarges text or reads it aloud.

- Utilize Peripheral Vision: Learn techniques from low vision specialists to make better use of your remaining side vision.
- Seek Support: Connect with low vision rehabilitation services or support groups.
- Find helpful tools: Visit Our Recommended Solutions
When to See Your Eye Doctor
- Regular Exams: Continue getting comprehensive dilated eye exams as often as your doctor recommends (usually yearly for seniors).
- Report Changes Immediately: If you have AMD, promptly report any new or worsening symptoms (like increased blurriness, more distortion, or new dark spots) to your eye doctor. Early detection and treatment, especially for Wet AMD, are crucial.
- Use an Amsler Grid: If recommended by your doctor, use an Amsler grid at home regularly to monitor for changes in your central vision.
Moving Forward with AMD
An AMD diagnosis requires adjustments, but it doesn’t mean the end of an active life. By understanding the condition, working closely with your eye care team, exploring treatments, and utilizing low vision aids and strategies, you can continue to live fully.
Elderly Care First is here to provide ongoing information and support for seniors and caregivers navigating AMD and other age-related eye conditions.





2 Comments